Possible Trigger of Crohn’s Disease Discovered: Dysfunctional Mitochondria Disrupt the Gut Microbiome
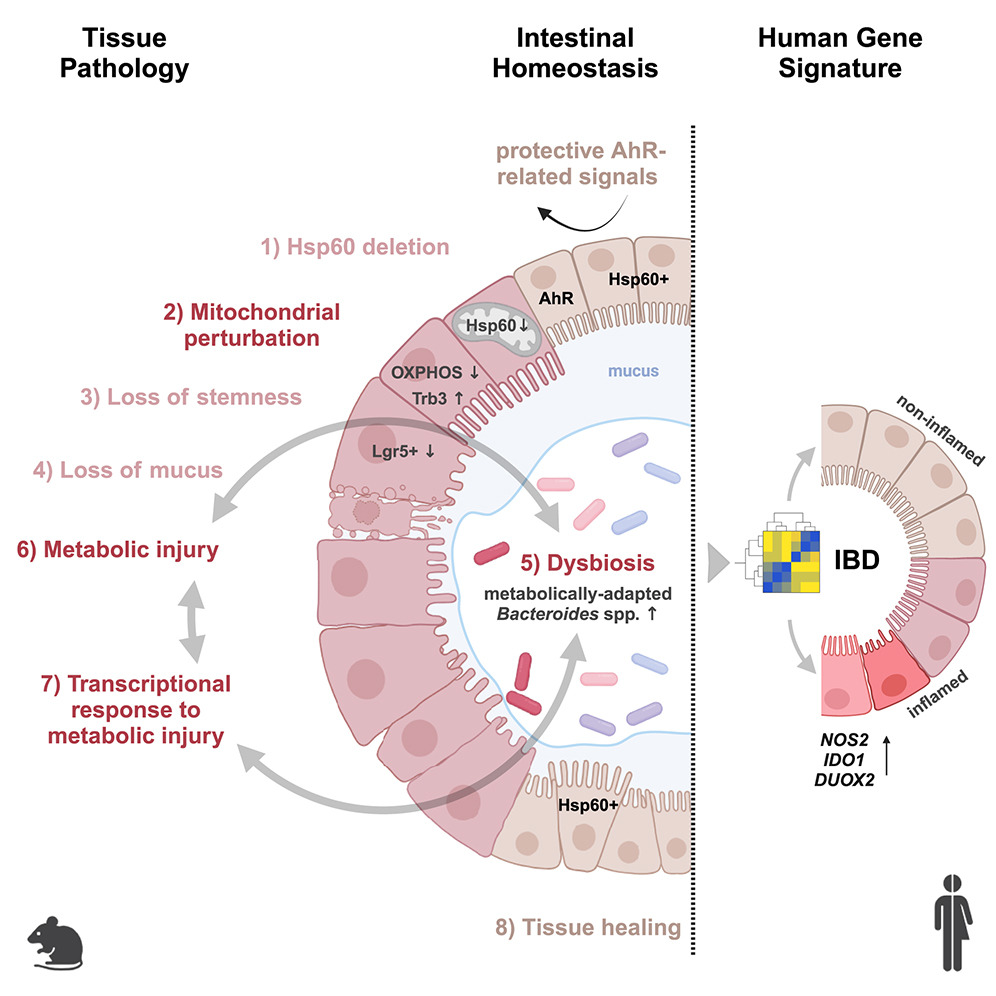
A team led by Prof. Dr. Dirk Haller at the Technical University of Munich (TUM) has uncovered a crucial link between mitochondrial dysfunction and Crohn’s disease (CD), a chronic inflammatory condition. Their study, published recently, shows that defective mitochondria trigger intestinal epithelial damage and lead to significant changes in the gut microbiome, offering new insights into the disease's pathogenesis.
Mitochondrial Disruption and Its Impact on the Gut
Crohn’s disease, characterized by symptoms such as chronic diarrhea, abdominal pain, and fever, has long been associated with alterations in the gut microbiome. While the root causes of Crohn's disease remain unclear, disruptions in microbial communities within the intestines are considered a potential trigger for the condition. However, until now, the mechanisms driving these changes have not been well understood.
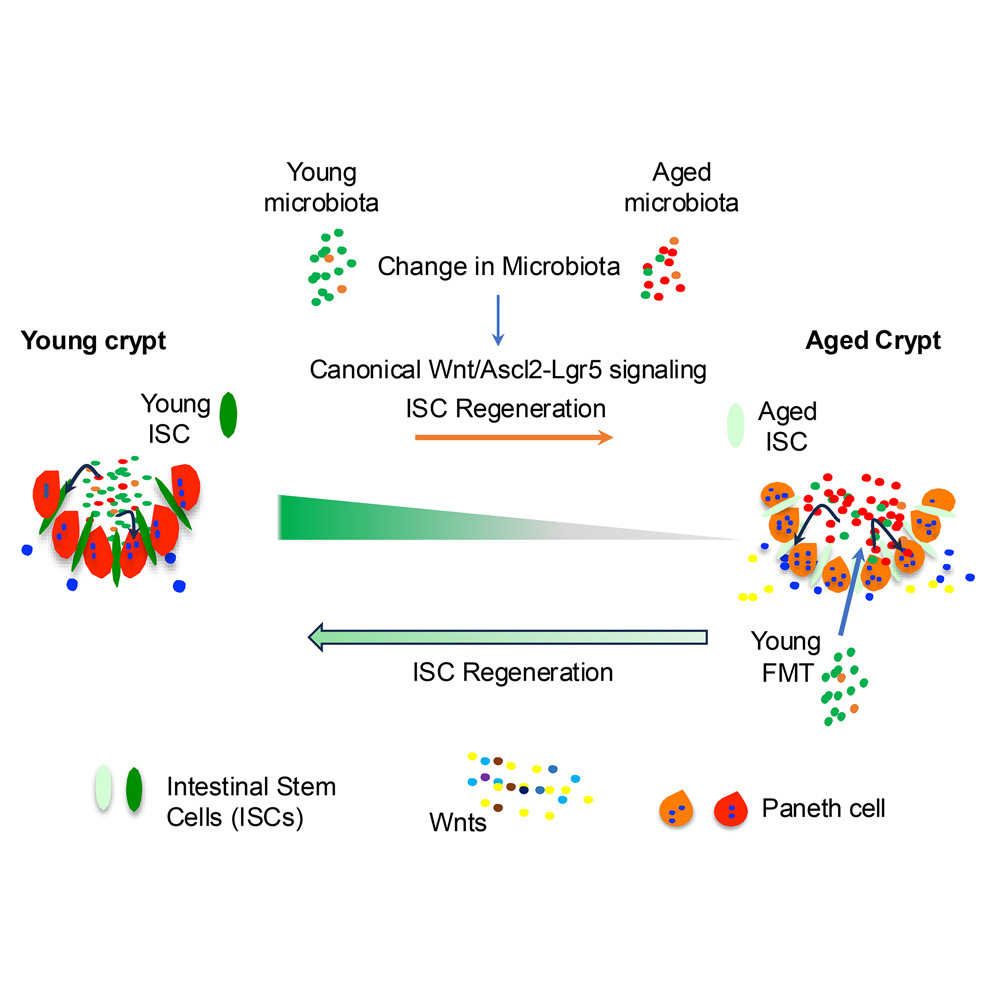
Prof. Haller’s research team sought to understand the interplay between mitochondrial function, the gut microbiome, and the intestinal epithelium—the layer of cells lining the inside of the intestine. Mitochondria, known as the cell's powerhouses, are responsible for converting nutrients into energy. They also play a vital role in cellular metabolism and function, including the health of the intestinal cells.
Key Findings of the Study
The researchers hypothesized that mitochondrial dysfunction could influence the gut microbiome. To test this, they induced mitochondrial defects in mice by deleting a gene segment responsible for producing Hsp60, a protein critical for mitochondrial function. The results were striking:
- Tissue damage in the intestinal epithelium similar to that observed in Crohn’s disease patients was detected.
- Gene activation patterns typical of Crohn’s disease were identified.
- Most importantly, disruptions to mitochondrial function were shown to cause significant shifts in the microbiome composition.
This marks the first time that scientists have demonstrated a causal relationship between mitochondrial dysfunction, intestinal damage, and changes in the microbiome, providing a clearer understanding of how mitochondrial health impacts gut inflammation.
These groundbreaking findings may have important therapeutic implications. Currently, treatments for Crohn’s disease focus on managing symptoms with anti-inflammatory drugs. However, Prof. Haller emphasizes the potential for novel treatments aimed at repairing mitochondrial function. "The big hope is to find active ingredients that would restore the functionality of disrupted mitochondria, essentially repairing them. This would help limit intestinal damage and the chronic inflammation processes that follow," says Prof. Haller.
The study suggests that targeting mitochondrial pathways or addressing the connections between the microbiome and mitochondria could lead to more effective treatments for inflammatory diseases like Crohn’s disease.
A Step Toward Better Therapies
As the research progresses, there is optimism that new drug developments will emerge that specifically target these mitochondrial and microbiome interactions, opening the door for more precise and impactful treatments for those suffering from chronic inflammatory conditions.
© Photo Credits: Urbauer, Elisabeth et al. Cell Host & Microbe (2024)